Dr. Phil Zeltzman’s Blog
The Devastating Impact of Poaching in South Africa and Zimbabwe
| I was very fortunate to recently visit South Africa and Zimbabwe after a veterinary conference. Since 100% of the pet owners we meet are animal lovers, I thought I would share some information and pictures about his incredible trip. |

Poaching remains one of the most critical threats to wildlife across the globe.
South Africa and Zimbabwe are two countries where the illegal hunting and capturing of wild animals are especially severe.
From rhinos to elephants, countless animals are suffering, and some are disappearing, due to illegal hunting, killing, and capturing.
Let's explore the various types of poaching, the reasons behind them, their devastating effects on animal populations, and the actions being taken to combat them.
By better understanding the urgency of the situation, we can all become part of the solution.

What are the different types of poaching?
Poaching isn't a one-size-fits-all threat.
It occurs in various forms, each with its unique impact on wildlife:
1. Killing for horns & tusks: commercial poaching is the most notorious form of poaching.
It's the illegal hunting of elephants and rhinos for their ivory tusks and horns, respectively.
These animals are killed brutally for their valuable body parts, which are then sold on the black market.
Rhino horns, for example, are prized in traditional medicine, especially in some Asian countries, despite having no proven medicinal benefits.
Why? Because the horn of a rhino is made of keratin. Keratin is the same protein that makes up human fingernails and hair.
So someone truly interested in the “medicinal” benefits of rhino horns could save a bundle – and lives – by eating their hair and biting their nails...
Rhino horns can fetch prices as high as $27,000 to $45,000 per pound ($60,000 to $100,000 per kg) on the black market.
When you know that a single horn can weigh 2.2 to 6.6 pounds (1-3 kg), you understand that this is life-changing money.
It gets even better (or worse): most rhinos have 2 horns, which doubles the bounty!
Bottom line: rhino horns are one of the most valuable substances on earth.
Below is the picture of the rhino’s skull that has been dehorned illegally.

2. Killing for food: This is called subsistence poaching.
In many rural communities in South Africa and Zimbabwe, wildlife is hunted for what is called "bushmeat."
This is due to food insecurity or economic desperation.
While some of this hunting is legal, the demand for wildlife as a food source can also lead to illegal poaching, depleting animal populations and threatening biodiversity.
3. Capturing live animals: Another form of poaching involves capturing wild animals alive for the illegal "pet" trade or for use in circuses and tourist attractions.
This is especially prevalent for species such as parrots, monkeys, and reptiles.
Animals are often taken from their natural habitats and transported under horrific conditions, causing immense suffering – and death.
Taking care of these animals is not easy. Surgeons deal with a specific type of fractures (“pathological fractures”) due to a lack of calcium and poor feeding habits.
Why is poaching so enticing?
The reasons behind poaching are complex and vary by region.
Some of the key drivers include:
- Poverty and economic incentives: Many poachers come from poor communities, where poaching is seen as a quick way to make money. Rhino horns, as mentioned, can fetch astronomical prices on the black market.
- Demand for animal products: There is demand for animal products like ivory, rhino horn, and skins, especially in international markets. These products are often viewed as status symbols, driving illegal trade.
- Weak law enforcement: In some areas, the lack of effective law enforcement and the corruption within local governments makes it easier for poachers to operate with little fear of consequences. These are gigantic and ruthless territories that are difficult to protect.
Which animals are affected by poaching?
The most commonly poached animals in South Africa and Zimbabwe include:
- Rhinos: Both white and black rhinos are heavily targeted for their horns. Poaching has decimated rhino populations in both countries.
- Elephants: Elephants are poached for their ivory tusks, a practice that has caused a dramatic decline in elephant numbers in Southern Africa.
- Big cats: Lions and leopards are also poached, primarily for their pelts, claws, and teeth, and sometimes due to conflict with farmers.
- Antelopes and other mammals: Species like kudu, impala, and wildebeest are sometimes poached for meat, especially in rural areas, though they are also targeted for their horns. And they can be found in supermarkets...

What are the consequences of poaching on animal populations?
The consequences of poaching are severe.
In South Africa, the rhino population has dropped by more than 70% in the past decade, due to poaching.
Similarly, elephant numbers have been severely impacted, in South Africa and Zimbabwe, where the illegal ivory trade continues to thrive.
The loss of these species not only affects the ecosystems they inhabit, but also threatens the economic stability of local communities that rely on tourism.
Without rhinos and elephants, many national parks lose their appeal to international tourists, which can have devastating economic consequences.
That's the cruel irony of the situation: some communities kill animals for short-term gains – to survive - without seeing the long-term consequences.
How does poaching happen?
Poaching is a highly organized crime in many cases.
Often, poachers are part of well-established organizations that use sophisticated methods to track, hunt, kill, and transport animals.
Here's a glimpse into how poaching operations typically unfold:
- The hunt: Poachers use guns, snares, or poison to kill animals.
- Processing: Once the animal is killed or captured, the horns, tusks, or other valuable parts are harvested. Nothing is as heart-wrenching as a dead, tusk-less elephant, or a dead, dehorned rhino, left behind to rot.
- Transportation: Animal parts are often smuggled across borders or shipped internationally to reach black market buyers. This illegal trade is typically carried out by criminal networks.
What is being done to fight poaching?
Both South Africa and Zimbabwe have taken significant steps to combat poaching, but there is still much work to be done:
1. Anti-poaching units: National parks and reserves employ anti-poaching teams that work tirelessly to protect wildlife. These units often include armed rangers who patrol vast areas and confront poachers directly.

2. Technology and surveillance: Advancements in technology, such as drones and satellite monitoring, have enabled conservationists to track animal movements and detect poaching activity in real-time.
3. International cooperation: Countries, Non-Governmental Organizations (NGOs), and international organizations are working together to curb the illegal wildlife trade. This includes sharing intelligence, conducting joint operations, and strengthening laws related to wildlife protection.
4. Community engagement: Some efforts are focused on educating local communities and providing alternative livelihoods to reduce the reliance on poaching. Programs aimed at improving local food security and economic opportunities are promoted to create sustainable, long-term solutions.
What can animal lovers do?
You don't have to be in South Africa or Zimbabwe to make a difference.
Here are a few ways you can help:
- Donate to anti-poaching organizations: Support groups like the World Wildlife Fund (WWF), African Wildlife Foundation, or Rhino Rescue to fund efforts against poaching.
- Raise awareness: Help me spread the word. Please share this blog with other animal lovers. Tell them about the effects of poaching and the importance of conservation. The more people know, the more pressure can be placed on governments and corporations to act.
- Advocate for stronger laws: Get involved in campaigns advocating for stronger anti-poaching laws and stricter enforcement of wildlife protection policies.
- Be a conscious consumer: Never purchase products made from ivory, rhino horn, or any animal body parts for that matter. Supporting sustainable and ethical businesses helps combat the demand for poached wildlife.

Poaching is a complex and heartbreaking issue, but it is one we can all help solve.
By raising awareness, supporting anti-poaching initiatives, and making ethical choices, we can help protect the incredible wildlife of South Africa and Zimbabwe.
The battle against poaching is far from over, but with collective action, we can ensure that these iconic species do not disappear from our planet forever.
We can't help your rhino, but if you would like to learn how we can help your cat or dog with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Eye to Eye with Royalty
| I was very fortunate to recently visit South Africa and Zimbabwe after a veterinary conference. Since 100% of the pet owners we meet are animal lovers, I thought I would share some information and pictures about his incredible trip. |

When Malema swiftly moved from his tracker’s seat, on top of the hood of the jeep, to the safety of the passenger seat, we knew that danger was near.
The group went quiet in anticipation, staring at the road ahead.
Suddenly, two majestic male lions appeared, lounging in the middle of the road!

We held our breath, in complete disbelief. After all, this was our very first outing!
The lions just sat there, pretending to ignore us.
At one point, one rolled on his back, like a household cat.
700 pictures later, the lions decided they were bored of being the center of attention.
They got up, and peacefully walked around the jeep, one on each side, staring at us with curiosity.
They moved with effortless grace, with a silent, powerful stride. The lion on the right locked eyes with me. It lasted a second, but I will never forget it. He was within 3 feet of me.

After a few moments, the lions disappeared back into the bush.
We sat in stunned silence, hearts pounding, trying to process what just happened.
It was an unforgettable encounter.
It was a reminder of the wild’s power and the incredible privilege of witnessing such beauty.
We can’t help your lion, but if you would like to learn how we can help your cat or your dog with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
The Cheetah’s Breakfast
| I was very fortunate to recently visit South Africa and Zimbabwe after a veterinary conference. Since 100% of the pet owners we meet are animal lovers, I thought I would share some information and pictures about his incredible trip. |

The morning sun cast a golden glow over the parched South African bush as our safari jeep crept along a dirt road.
The air was thick with anticipation, every sense heightened in search of elusive wildlife.
Suddenly, our tracker raised a hand, signaling silence.
A few feet ahead, completely hidden by leafless bushes, we eventually recognized the unmistakable silhouette of a cheetah.

Her sleek, muscular body lay close to the ground, head bent down as it feasted on the lifeless form of a young gazelle.
This was a rare find!

This was obviously an incredible discovery made by our tracker.
We approached cautiously, keeping a respectful distance.
The cheetah was entirely focused, tearing into the gazelle with efficiency, each rip of her teeth reminding us of the raw survival instinct governing life here.
It was hard to watch as animal lovers, yet captivating and exceptional.
Our cheetah paused, lifting her head to scan her surroundings with piercing amber eyes, mouth streaked red.

The powerful predator looked more magnificent up close than I could have ever imagined, a blend of grace, innocence and ferocity.
As we watched in complete disbelief, the bush was hushed, except for the occasional crunch and pull of the cheetah’s meal.
The scene felt both brutal and beautiful. It’s the circle of life. No gazelles, no cheetahs…
After a few minutes, the cheetah looked up again, locking eyes with us.

We felt like intruders in a private ritual.
The cheetah resumed her feast, undisturbed by our presence, while we sat in quiet awe, touched by the primal intimacy of witnessing one of Earth’s most powerful hunters in its element.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Why did my vet stick a finger up my pet’s XXXX?

I’ve never had this experience, but I’ve heard from colleagues that some pet owners were completely shocked when they stuck their finger in their dog or their cat’s anus.
(granted, it’s not a fun part of the exam for anybody involved!)
There are many excellent reasons for doing it.
In fact, I strongly believe it should be part of any complete physical exam.
In larger, well-behaved dogs, this can be done awake.
In fractious or small pets, it absolutely should be done under sedation.
Here are 13 reasons a veterinarian might perform a rectal exam on a cat or a dog, regardless of gender:
1. To assess or empty anal sacs
Anal sacs are a complete nuisance!!!
Most pets empty them spontaneously when they poop.
Some do not however, and they need a bit of veterinary help when they get too full.
The glands need to be emptied or “expressed.”
Your vet may also check for an infection or a tumor in the anal sacs.
Removing one of both is a common surgery in our practice, both for infection and mostly tumors.
2. To detect a mass in the rectum
Pets can have tumors, either cancerous or benign (like a polyp).
3. To evaluate the prostate
In male pets, the prostate gland can become enlarged and can cause problems peeing.
4. To investigate rectal bleeding
A pet can have blood in their stools for multiple reasons.
Fresh blood could come from the rectum, so that justifies doing a rectal exam.
5. To confirm a hernia
Dogs, mostly intact males, can have a hernia called a perianal hernia.
A simple rectal exam will confirm it.
Repairing it is a fairly common surgery we perform.

6. To detect a foreign body
Occasionally, a foreign body will travel all the way from the mouth, through the stomach and the intestine, and may strangely get stuck in the rectum.
I remember a sewing needle that did exactly that.
I was able to confirm it and remove it through the rectum.
7. To assess fractures of the pelvis
Even better, some fractures can be realigned during a rectal exam.
8. To assess “rectal tone”
A decreased muscle tone (or strength) of the anus can be a sign of neurological issues.
This can happen in paralyzed dogs or dogs who are incontinent.
9. To treat a rectal prolapse
A rectal prolapse means that part of the rectum sticks out of the anus.
The 1st attempt at fixing it should be to try to push it back in place.
10. To diagnose urinary issues
During a rectal exam, a vet can feel the urethra (the tube coming out of the bladder) for abnormalities or blockages, for example if a bladder stone moved downward.
Rarely, a tumor can be felt.

11. To check the area before or after surgery
Before and after any surgery involving the rectum, the anus, or the anal sacs, a rectal exam will typically be performed before and after surgery.
12. To assess narrowing of the rectum
The rectal passage may have a stricture or stenosis, which would cause defecation issues.
13. To check for fistulas
Some dogs, such as German shepherds, can have abnormal connections (i.e. fistulas) between the rectum and the skin.
So there you go.
There are probably other reasons, but the 13 above are the most common reasons a vet may stick a finger up there.
This simple test can save your pet’s life!
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified
Pete Baia, DVM, MS, DACVS

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Will my pet be normal after surgery?

This is a surprisingly common question from clients.
I will explain my standard answer, then share answers from a few surgeon colleagues when they get the same question from their own clients.
My answer
I typically provide 3 answers:
1. “I’m not a magician, I can’t promise you normal.”
I also typically say: “I can’t promise you your dog will be the agility champion of the universe.”
The goal is to end up with a pet who is comfortable, happy, and able to have normal activities. For a family pet, this includes: running after a ball, jumping on the couch, sleeping on the windowsill, jogging around the block, playing with kids and other pets, etc.
Anything above that is icing on the cake.
Now, we also work on sporting dogs, who need to do much more for a living: police dogs, search and rescue dogs, hunting dogs etc.
In such cases, although I never promise the moon, we mostly need to modify the rehab portion of the postop care for orthopedic patients to get them back to peak performance.
Athletes clearly near more rehab than family pets.

2. “I’m responsible for 10% of the outcome”
Now, of course, the answer greatly depends on the diagnosis.
The outcome of surgery for aggressive cancer in a 15 year old cat, cannot possibly be the same as the outcome of a fracture repair in a healthy 6 month old pup.
Then I explain, tongue in cheek: “I’m responsible for 10% of the outcome of surgery. You’re responsible for 90% of it.”
Why? Isn’t the surgeon entirely responsible for the outcome of their surgery?
I wish it were that simple.
In a straight-forward case, like ACL surgery or a simple fracture repair, I know exactly what is going to happen in surgery and I can pretty much predict the end-result, from the moment the patient walks in the clinic, to the moment they go home.
However…
3. “I cannot control what happens at home”
Before surgery, we explain, at length, how strict the postop care needs to be.
We explain the importance of keeping the plastic cone on at all times to prevent licking and chewing the incision, and to avoid opening it up, or causing an infection.
We explain the importance of keeping the pet strictly confined, locked up in a small area.
Dogs should always be on a short leash, for a few minutes, to eliminate outside.
In some patients, especially fractures in young pets and after FHO surgery for hip issues in cats and dogs, we insist on the vital importance of physical therapy.
But it doesn’t mean that all of the instructions are followed.
As I always say, “Pets are pets and people are people.”
Now, fortunately, the vast majority of clients are incredibly dedicated and follow the instructions.
And they are typically rewarded with a great outcome.

My hope
In a straight-forward case, like ACL surgery or a simple fracture repair, my expectation is that 95% of my patients should get to 95% of normal.
Why not 100%?
For the reason explained above. I can’t control what happens at home.
When I feel that the pet owner has a good sense of humor, I also say: “I get the easy part: the surgery. You get the hard part: the recovery at home.”
To get a better idea of what surgeon colleagues tell their clients, I asked a few friends how they answer that question: “Will my pet be normal after surgery?”
Answer from a surgeon in New York
Dr. Kathy Collins, a board-certified traveling surgeon serving western New York State, tells her clients:
“I can’t make your pet normal, but I can make them much better. How much better depends in part on how well you do your tasks at home: rest and rehab. My job is the technical part. Yours is the hard part.”
Answer from a surgeon in Oklahoma
Another surgeon tells his clients: “As a medical professional, I can’t use words such as “normal,” “cure” or anything that implies a guarantee.
To the human eye, most patients may appear normal after a few months. But I can tell you as someone who has had ACL surgery before, I still have some bad days even 5 years later.
Can I make a patient as normal as before the injury? No.
But I can offer less pain. I would choose that for my own pet over and over again.”
Answer from a surgeon in Florida
Dr. Rob Fernand, a traveling surgeon based in Plantation, FL, tells his clients:
“After a fracture repair or a torn ACL, a pet will never be normal again. Our goal is to get them to run and jump and play as if nothing ever happened. But they may have good days and bad days.
After ACL surgery specifically, he says: “95% of the time you shouldn’t see them slow down or limp. But the other 5% is when you may see some stiffness in the morning or after a long day in the park. They will never have a “normal” knee again.”
See a trend here? We basically say the same thing!
I should also mention that we still can help these pets long-term. Depending on the situation, we can provide life-long arthritis supplements, and we can use pain medications when they have a bad day.
So the good news is that if the surgeon does their job, and the pet owners follow instructions, and the pet behaves at home, we pretty much all expect that 95% of patients should get to 95% of normal.
If they are better than that, then maybe you should send some chocolates & Champagne to your surgeons and their nurses!
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
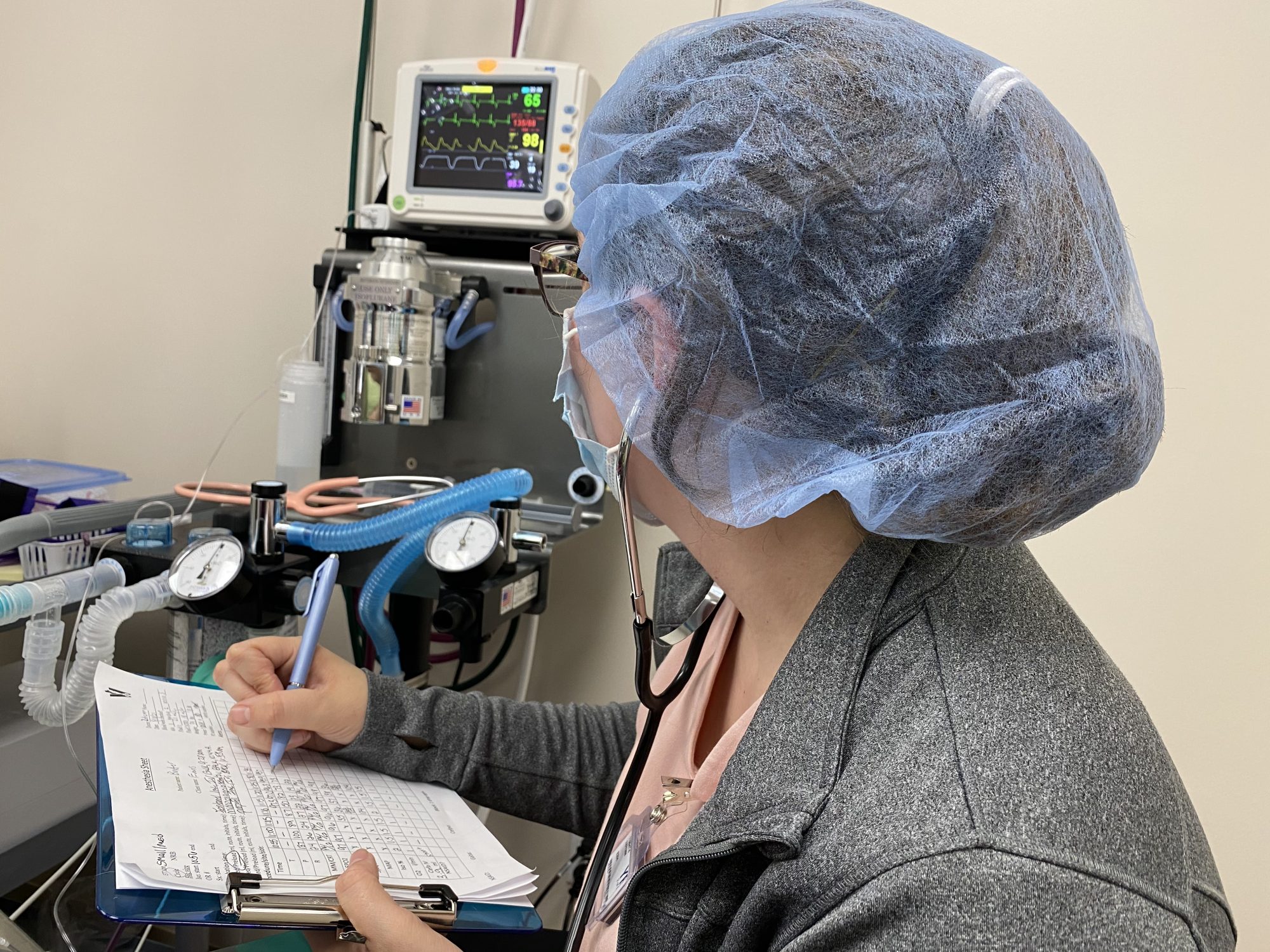
3 secrets of safe anesthesia

Most owners are afraid of anesthesia, although it’s incredibly safe.
The risk of dying under anesthesia, taking into account the healthiest patients as well as the sickest, is a fraction of 1%.
Still, we all wish we would have zero deaths related to anesthesia.
One way to make sure your pet will be safe under anesthesia is to understand what happens, or should happen, during the 3 steps of any anesthesia.
1. How to keep your pet safe before anesthesia
We routinely (i.e. 100% of the time) take at least 4 steps to ensure a patient is a good candidate for anesthesia.
- Blood work. This allows us to make sure your pet can carry oxygen (enough red blood cells), can clot (enough platelets), can fight infection (enough white blood cells), has a healthy liver and healthy kidneys, has normal electrolytes, etc.
- We perform a physical exam.
- We assess the patient’s individual anesthesia risk (called the “ASA” risk).
- We discuss the anesthesia and pain management protocols as a team (surgeons and nurses) so they are adapted to the patient and their particular surgery. For example, we use a different protocol for pets with kidney, liver and heart disease. We use a special protocol for dogs (and cats) with a flat face (English Bulldogs, French Bulldogs, Boxers etc.). We use a different protocol for diabetics and pediatrics.
As we always say, “every patient is different.”

2. How to keep your pet safe during anesthesia
In the vast majority of patients, fortunately, everything goes perfectly well.
Occasionally, we run into problems: the heart rate drops or increases, the bloodqqq pressure drops or shoots up, the patient has difficulty breathing…
Fortunately, in the vast majority of patients, we can quickly get the situation under control.
But we never take anything for granted, so every single patient has a dedicated anesthesia nurse, whose only mission is to keep her patient safe.
Anesthesia monitoring means the patient is monitored by a fancy machine.
It allows us to monitor the heart (EKG), blood pressure, oxygen level (pulse oximetry), temperature, respiratory rate and CO2 levels (capnography).
And of course, every patient has an IV catheter to receive IV fluids, antibiotics, and pain medications.
3. How to keep your pet safe after anesthesia
A common misunderstanding is to believe that once a patient is out of the OR and awake, they’re safe.
The reality is that most deaths related to anesthesia occur AFTER surgery, not during.
Over half of patient deaths occur within 3 hours after the end of anesthesia.
That’s the reason why we continue to monitor our patients closely after they wake up from anesthesia.
We monitor their breathing, heart rate or pulse, comfort level, and more.
We’re also a tiny bit obsessed with keeping our patients warm.
The sicker the patient, or the higher the anesthesia risk, the more intensive postop supervision should be.
This is especially true in cats and dogs with a flat face (brachycephalic breeds).
So if your pet needs anesthesia, which question should you ask?
Here are some questions you should feel perfectly comfortable asking before your pet goes under anesthesia:
- What testing will be performed before anesthesia to make it safer?
- Will my pet be supervised by a nurse throughout anesthesia?
- What kind of monitoring do you provide during anesthesia?
- What kind of supervision will my pet have while recovering from anesthesia?
- Is there overnight care?
Bottom line: most pet owners ask questions about the surgery.
I think they should ask more questions about anesthesia.
Your pet’s well-being depends on it.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!