Dr. Phil Zeltzman’s Blog
What cardio-vascular complications can happen during anesthesia? (part 2)

This is part 2 of our anesthesia complications blog series. You can read part 1 here.
The bad news: Every anesthesia carries some risk.
The good news: most complications are minor, and quickly and easily fixable.
Let’s go over some cardio-vascular anesthesia complications.
1. Bradycardia
Bradycardia is a fancy word that means that the heart rate is too low.
Common causes include:
- The anesthesia is too deep. The simple solution is lower the amount of anesthesia gas.
- The body temperature is too low. This is something we fight from start to finish.
- Electrolyte abnormalities. Most commonly, it is related to potassium being too high in the blood. This can happen in pets with a blockage that prevents them from urinating. We try to correct that before anesthesia even starts.
- Morphine-like drugs. That’s a common side-effect. If the heart rate is too low, we can use drugs to increase it.
2. Tachycardia
Tachycardia is the opposite of bradycardia, so it means that the heart rate is too fast.
The most common causes include:
- The anesthesia is too low. The simple solution is to give a bit more.
- Pain. We would then give even more pain medications than we typically provide.
- Some diseases, such as a tumor in the adrenal gland. This would be temporary, until the tumor is removed, and we can use drugs to lower the heart rate if needed.
3. Hypotension
Hypotension means that the blood pressure is too low, just like in some people.
The most common causes include:
- Severe bleeding. The solution would be to give more IV fluids or possibly a blood transfusion.
- Cardio-vascular diseases. Hopefully, this is something we know ahead of time, and can treat with meds before anesthesia starts. We sometimes use different drugs for anesthesia. We are also less generous with IV fluids so we don’t overload the heart.
- The anesthesia is too deep. We would then provide less anesthesia gas.
- Some drugs. We can give IV fluids or drugs that can correct that.
- Some conditions. For example, mast cell tumors in the skin can release a substance that causes the blood pressure to drop. We routinely use drugs before anesthesia to prevent this from happening.

4. Hypertension
Hypertension is the opposite of hypotension, so it means that the blood pressure is too high, just like in some people. The most common causes include:
- The anesthesia is too light. So we would simply give more anesthesia drugs.
- Some diseases. For example, a type of tumor of the adrenal gland (pheochromocytoma) can release a substance that causes the blood pressure to spike. There are drugs we can use to lower the blood pressure.
5. Arrhythmias
Arrhythmia is a fancy word that means that there are abnormal or extra heartbeats.
The most common example is extra heartbeats during “bloat” (twisted stomach) or spleen surgery.
This usually resolves eventually with drugs and time.
Fortunately, the risks of severe complications are small, and most complications can be solved quickly.
The key is to have good monitoring equipment, and above all, experienced anesthesia nurses.
Every patient we anesthetize has a dedicated anesthesia nurse whose only job is to keep her patient safe.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
What breathing complications can happen during anesthesia? (part 1)

Many clients are scared of anesthesia. And rightfully so. It’s a big deal !!!
As we often say, “There are routine surgeries, but there is no routine anesthesia.”
Yet, the risk of dying under anesthesia for a cat or a dog is, on average, less than 0.25%.
While every death is an absolute tragedy, this number is incredibly low.
The risk is even lower in healthy patients, and a bit higher in very sick patients.
Still, this number is very low, which means that anesthesia is overall very safe.
This will be a 4 part blog to explain some complications that can occur during and after anesthesia. We will start with breathing complications.
When a pet goes under anesthesia, they lose consciousness – by definition.
Occasionally, their lungs don’t quite do what they’re supposed to.
So a few complications can happen.
Fortunately, they are often short-term and fixable.
1. Apnea
You may have heard this word when people talk about holding their breath, for example underwater.
The same thing can happen during anesthesia: the pet stops breathing.
It can happen to any patient, most often at the very beginning of anesthesia, and occasionally during surgery.
Should that happen, the solution is simple: the nurse would “breathe for the patient” by squeezing the anesthesia bag, to give some oxygen to the patient.
It usually resolves quickly.
It can also happen because the patient is “too deep”, which means that (s)he received too much anesthesia drugs or gas.
This is also fixable by decreasing the amount of anesthesia gas given.
2. Hypercapnia
A fancy word that means that the pet has too much CO2 (carbon dioxide) in their system.
There are multiple reasons, such as lung disease or being overweight.
Again, the nurse would assist the patient to help them breathe more CO2 out.

3. Hypoxemia
This is a medical term that means that the pet doesn’t have enough oxygen onboard.
This is a big deal.
It can occur for a number of reasons: not enough red blood cells (anemia), lung disease (including big tumors), chest diseases (free air or fluid in the chest etc.).
Fortunately, this is very rare.
As you can see, the risks of severe breathing complications are small, and most complications can be resolved quickly.
The key is to have good monitoring equipment, and above all, experienced anesthesia nurses.
Every patient we anesthetize has a dedicated anesthesia nurse whose only job if to keep her patient safe.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
What to do about hip dysplasia?

Hip dysplasia is a fancy way to say that the hip joint did not form correctly.
The hip is a “ball and socket” joint. It is made of the ball of the femur or thigh bone (aka femoral head), and a socket or cup in the pelvis (aka acetabulum).
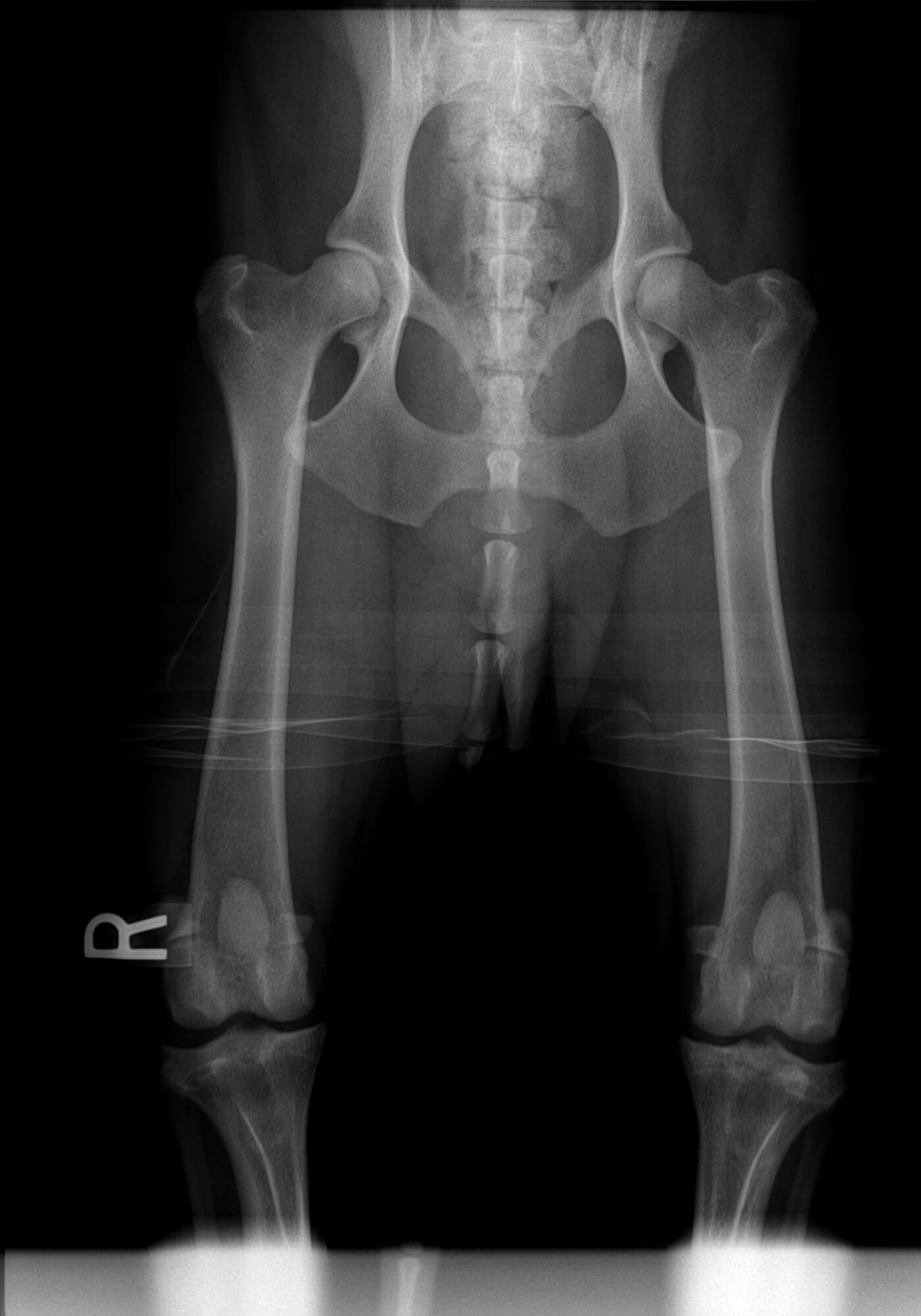
We typically think of hip dysplasia as a canine condition. In fact, cats can be affected as well.

Hip dysplasia can cause pain.
Young patients are typically painful because of stretching of the ligaments of the hip as the ball slips in & out of the socket.
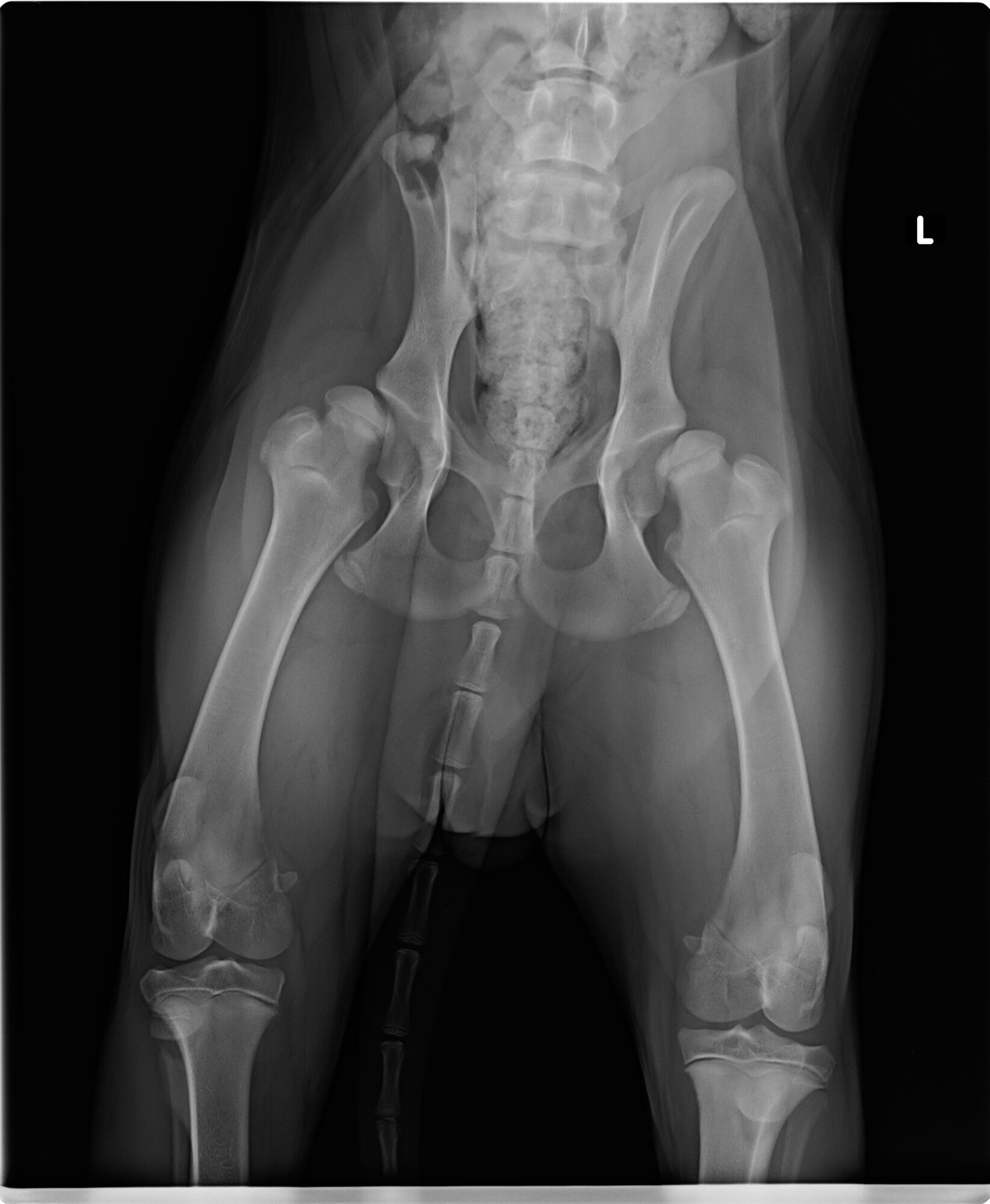
A very important point is that there is not always a good relationship between how bad X-rays look and how bad a patient feels.
In other words, patient A may have “horrible” hips on X-rays (meaning full of arthritis), yet may be functional and happy and able to run.
Whereas patient B may have “OK” hips on X-rays (meaning without much arthritis), but may act very painful.
As I always say, “I don’t treat X-rays, I treat pets.”Depending on the severity and the stage, there are many ways to help hip dysplasia patients.
The conservative way is to use all or some of the options we have discussed before to help arthritis: weight control or weight loss, arthritis supplements, arthritis diets, physical therapy, controlled exercise, pain medications etc.
The surgical way involves 4 mainstream options:
- Two “puppy” surgeries: Juvenile Pubic Symphysiodesis (JPS) and Triple Pelvic Osteotomy (TPO). They can only be performed in young patients who are very carefully selected. If a young patient is not a good candidate, then the following options will be more successful.
- and two “salvage procedures”: Femoral Head Ostectomy (FHO) and Total Hip Replacement (THR). Those can be performed at any age.
In cats, the most common option is the FHO, although a few surgeons have performed total hip replacements in cats.
Overall, hip dysplasia is a treatable condition.
It’s not a death sentence.
Make sure you get the right advice!
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
How can my pet have arthritis so young?
To answer this excellent question, let’s go over 3 classic, real-life scenarios.
Amber and the torn ACL
Amber, a 9 month old Lab, was presented for a torn ACL. An ACL can literally tear at any age, so we see it in puppies, young dogs, mature dogs and seniors. Even cats can occasionally have a torn ACL.
And we certainly can address them at any age.
Because of a bit of denial and back-and-forth between rest and pain medications, Amber’s surgery was delayed for a couple of months.
During that time, the body tried to patch things up by adding scar tissue and bone spurs around the knee. After surgery, I described her arthritis as severe. Yet she was only 11 months at the time of surgery!
Why? Simply because the knee had been wobbly for a long time, which gave the body plenty of time to try to patch things up – which it did poorly.

By the way, please note that when I say “arthritis”, it’s a bit of a simplification.
It may be a bit oversimplistic, but basically:
Arthritis = osteo-arthritis = Degenerative Joint Disease = DJD = bone spurs.
Sweetie and the dislocated kneecaps
Sweetie, a 6 month old kitten, was really struggling to run and jump like her sibling Simba.
She limped and was painful in both back legs.
Her issue? Both her kneecaps (or patellas) were dislocating (or dislocated, or luxated).
Because of a common misconception that cats don’t need their kneecaps fixed, surgery was delayed by 3 months.
After surgery, I described her arthritis as severe.
She didn’t have that many bone spurs, but her cartilage was discolored. Instead of being white, shiny and smooth, it was pinkish, dull and irregular.
Worse, it was partially gone under her kneecap and in the groove where the kneecap is supposed to stay.
The reason for the “bone on bone” (instead of cartilage on cartilage) is that every time the kneecap popped in & out of the groove, it mechanically damaged the cartilage.
It’s simple wear and tear.

Tank and hip dysplasia
Tank, a 9 month old Cocker spaniel, was in severe pain in both back legs. He was very painful in both hips. His problem? Severe hip dysplasia, which means that his hips were not formed properly.
Similar to Sweetie’s case, the ball popped in and out of the socket. Not only did it mechanically damage the cartilage (wear and tear), but as in Amber’s case, that abnormal motion also led to bone spurs.
The hip is a ball and socket joint.
Tank got pain relief thanks to a surgery that removed the ball part (Femoral Head Ostectomy or FHO).

As you now understand, the severity of the arthritis in Amber, Sweetie and Tank has nothing to do with their ages.
It has to do with their conditions, and the duration of the issue before surgery took place.
By doing surgery early on, we can’t fix the arthritis.
Surgery can however correct the actual problem, and slow down the progression of arthritis.
If you would like to learn more about how your pet can have safe surgery and anesthesia, contact us through www.DrPhilZeltzman.com
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified
www.DrPhilZeltzman.com

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
How do we monitor your pet’s anesthesia?

Vets have been able to dramatically decrease the death rate under anesthesia thanks to better anesthesia drugs and better monitoring.
What does monitoring mean?
Let’s review some techniques we use at our hospital to reduce the risks.
Please understand that not all practices have this equipment, for financial reasons mostly. As a general rule, we perform higher-risk and longer anesthesia and surgery, so we have an obligation to provide the best equipment available.
Vital signs
One of the many roles of the anesthesia nurse is to record the pet’s vital signs and numbers indicated by the devices described below: body temperature, blood pressure, heart rate, respiration rate, temperature etc.
This is critical to determine if there is a trend.
For example, is the blood pressure slowly dropping?
The surgeon is then alerted, and decisions can be made in a timely manner.
ECG
Most people have had an ECG (aka EKG), so most are familiar with the concept. An ECG measures the electric currents generated by the heart. It helps monitor the heart rate and rhythm. It allows early recognition of heart issues, such as arrhythmias (extra heart beats), which can then be treated appropriately.
Blood pressure
Blood pressure measurement is probably the earliest indicator of problems with anesthesia in pets.
Pulse oximetry
This is a way to estimate how much oxygen is being carried by red blood cells.
You may have been connected to such a device at the hospital.
This is the clip that is usually placed on your finger.
In pets, the probe is usually placed on the tongue.
Temperature
Anesthesia commonly reduces the body’s temperature.
We are obsessed with maintaining pets’ temperature, especially small ones.
Opening a body cavity (chest or belly) leads to losing even more body heat.
So we use several modalities to keep the temp up.
For example, every single patient gets a “Bair Hugger,” which is a warming blanket, in addition to a heating pad under their body.
It is important to warm patients up after surgery as well.
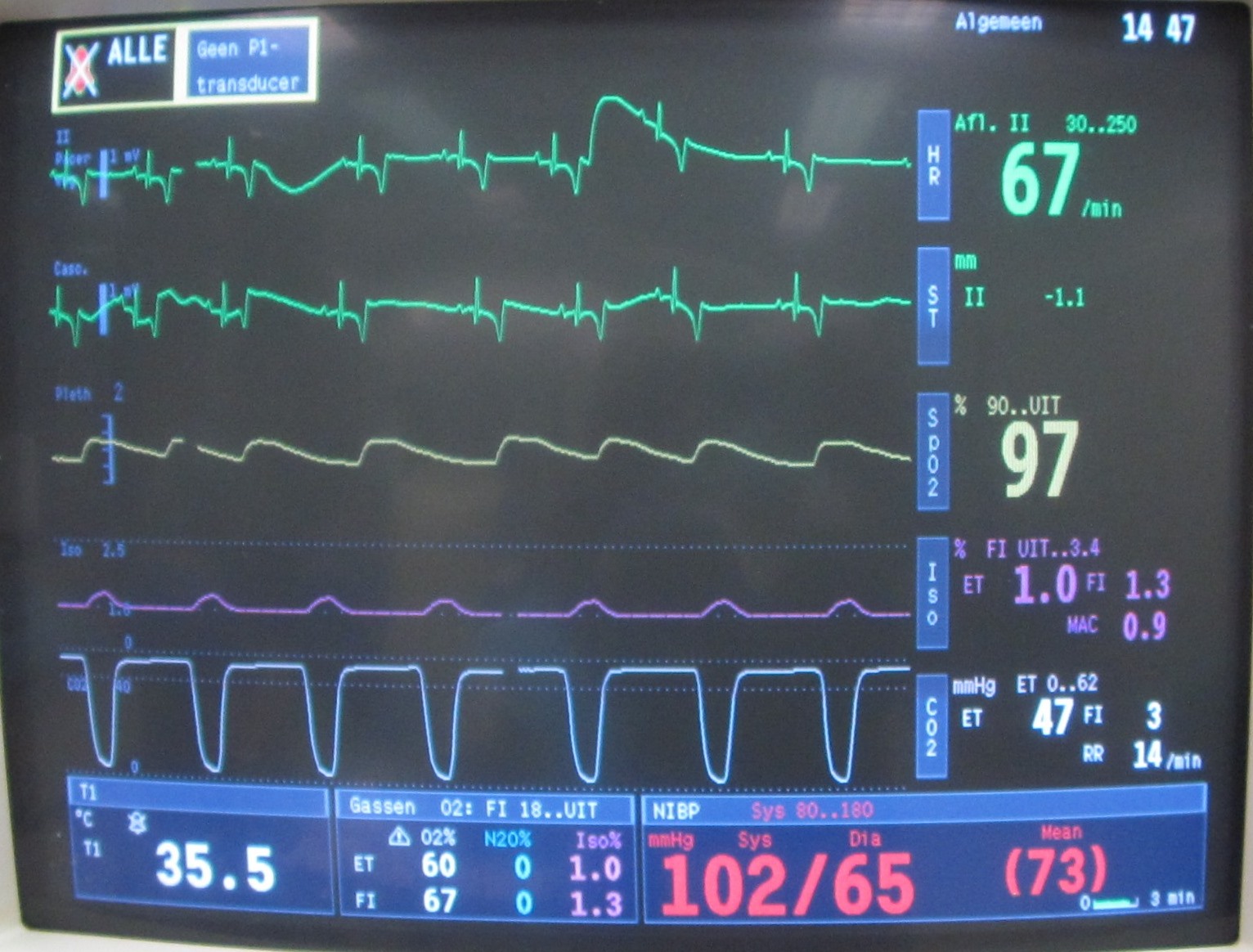
Capnography
This is a fancier machine, not routinely available in general practices.
It monitors the amount of CO2 (carbon dioxide) in the patient.
If it becomes too high, it means that the patient is not breathing enough to “blow off” the toxic CO2.
The anesthesia nurse would then help the patient breathe.
Such equipment undoubtedly helps us greatly improve the safety of anesthesia.
By far, my favorite way to monitor my patients is my skilled nurses.
The risk obviously depends on the patient and the type of surgery.
For example, spaying a healthy 6 month old Lab puppy is less risky that removing a 1 pound cancerous tumor from the liver of a 14 year old diabetic, seizure-prone poodle with heart and kidney disease!
That said, the OVERALL death rate under anesthesia is:
. 0.06 to 0.43% in cats;
. 0.11 to 0.43% in dogs
according to several studies conducted in the late 1990s.
As you can see, careful monitoring makes the anesthesia as safe as possible, so that we can reach our ultimate goals: a healthy pet and a happy pet owner.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!