Dr. Phil Zeltzman’s Blog
How risky is it to anesthetize super young pets?
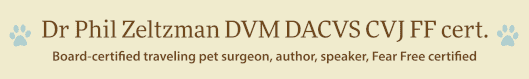
Rosalina, a 3 month old kitten.
Lukas, a 2 month old coyote.
Pup, a 3 WEEK old puppy.

What do these tiny patients have in common? They all needed a broken bone repaired. And they all super young.
Rosalina the kitten had a broken femur (thigh bone).
Lukas the coyote had a fractured humerus (arm).
Pup the puppy had a broken tibia (shin bone).
Their surgery was definitely challenging because of their soft bones. But the biggest challenge is really anesthesia.
Why is the risk of anesthesia in pediatric patients higher than in other patients?
Younger patients are at risk for hypoglycemia (low blood sugar), hypothermia (low temperature) and hypotension (low blood pressure).
Hypoglycemia
Younger patients have very little body reserves on board. So they are at risk for hypoglycemia (low blood sugar).
Patients who are old enough are often fasted at 8 pm the day before anesthesia.
In young puppies and kittens, we can’t do that, precisely to prevent hypoglycemia. Babies are typically allowed a small meal the morning of surgery.
Their blood sugar should then be monitored before, during and after anesthesia. If it’s too low, we can give sugar IV (in the form of dextrose) or by mouth (in the form of Karo syrup).

Hypothermia
Another struggle is keeping very small patients warm. All patients rapidly loose body heat under anesthesia. Super young patients are an even bigger challenge.
Of course, the solutions are well-known: warm air blankets, warm water blankets, IV fluid warmers etc.
These warming devices actually need to be put in action early and systematically to keep your pet safe.

Hypotension
Our pediatric patients may also have trouble with low blood pressure as a side effect of anesthesia.
Low blood pressure can be very dangerous if not corrected. Blood needs to appropriately move through the body to carry oxygen to all vital organs, such as the kidneys.
Decreased oxygen makes just about everything unhappy. It’s so important, that we monitor all of our patients’ vitals, including blood pressure, so changes can be identified early and corrected.
Blood work
Another way to decrease the risk of anesthesia is to run blood work. This helps us ensure that vital organs like the kidneys and the liver are healthy, and your baby can safely go under anesthesia. Of course, this applies to adults as well, and especially to seniors.
If the blood work does uncover an abnormality, it does not necessary mean that surgery will be canceled. However, it will often mean changing the anesthesia medications & postop pain medications used.
One specific thing we look for in young patients is abnormal numbers that could indicate an important condition called a liver shunt.
None of this information should change your mind about doing surgery. What it should do is educate you to make sure you and your vet can come up with the best plan for your baby, with the safest anesthesia and the smoothest recovery possible.
Hypoglycemia, hypothermia and hypotension are pretty straightforward to prevent when you are working with an experienced team. So don’t be shy about asking questions, so your super young pet is safe during anesthesia and surgery.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Who on earth wants surgery on their 23 year old cat?
I recently repaired a fracture on a 23 year old cat. Some of my nurses aren’t even that old! It’s a true story with a very happy ending.
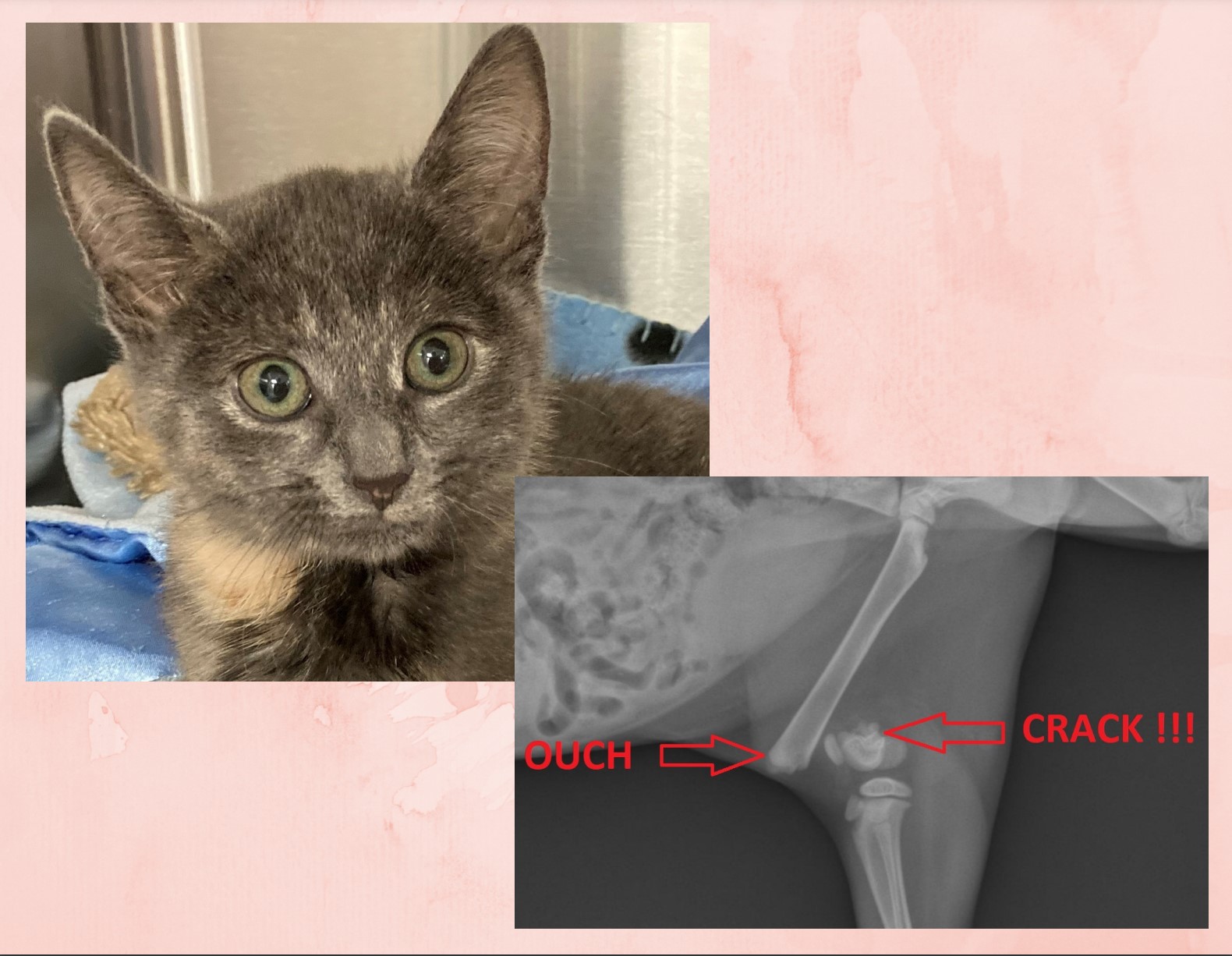
Basil, the 23 year old cat, had a broken tibia. The shin bone was broken in 3 main pieces. He went to the local ER, where his owner was told that he was too old and should be put to sleep.

That did not sit well with Basil’s owner. He may be 23 years old, but he was healthy otherwise, so why end his life? His owner contacted me regarding Basil’s situation. We agreed that it was ethical to perform surgery on him, since he was healthy otherwise, and we scheduled him for surgery.

Fixing the shattered bone required 1 pin, 1 plate, 4 wires, and 9 screws to repair! A bone graft was added to speed up healing. Surgery went well and sweet Basil recovered smoothly under the close supervision of his nurses.
At home, he was strictly confined for 8 weeks. At suture removal, after only 2 weeks, he surprised everybody by walking around using the leg very well.
And after 8 weeks, follow up X-rays showed that the bone had healed nicely and we could start to increase Basil’s activity.

And after one more month of that, Basil returned to his normal Grandpa life.
So what’s the moral of this story?
As I always say, “Age is not a disease.”
A few conditions need to be met for surgery to be a valid option in my opinion:
. The patient should be reasonably healthy
. The condition should be fixable.
. Quality of life should be good after surgery.
. The owner should be 100% on board.
Two months after surgery, Basil’s owner writes: “My sweet 23 year old cat is finally back on the couch with me. He is getting giant hugs. He’s really doing great. I really have no words to thank you enough.”
I don’t see why we should deny help to a patient who fulfills these criteria.
Basil’s owner certainly felt that way, and I am sure Basil did as well…
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
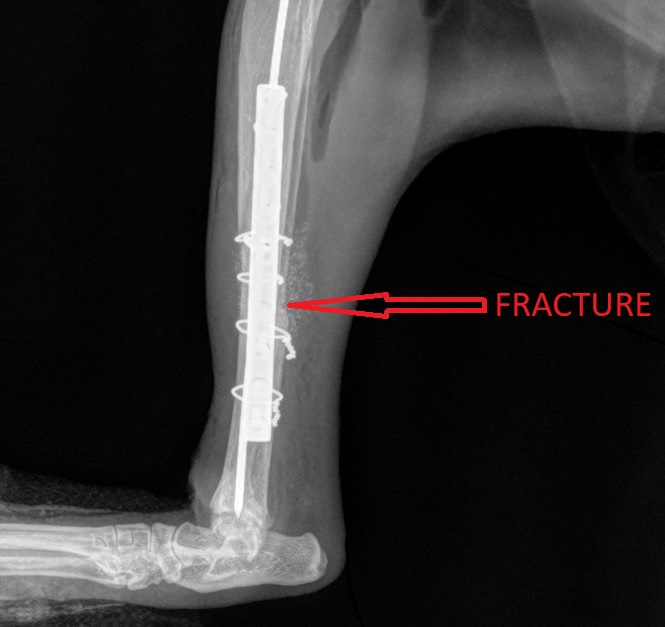
E Collars and Your Pet- Cone of Shame or Best Friend?
Ah, the dreaded “cone of shame…”
After any surgery, we strive to send your pet home with an incision that looks as nice as possible. The plastic cone or E collar (short for Elizabethan collar) was created to prevent licking. Without it, licking or chewing can cause irritation and discomfort.

At best, that may leave a hairless, discolored, ugly scar – for life.
Or it could lead to an open incision, that needs another surgery to close it up.
At worst, it can cause a serious infection.
| WARNING: some pictures below might be disturbing to some sensitive readers. |
Despite the stubborn urban legend that animal saliva speeds up healing, licking an incision is a sure way to slow down healing. The tongue, especially in cats, is so rough, that it can destroy healing tissue, and therefore delay healing.
Depending on the particular pet or level of discomfort, licking can lead to nibbling and chewing, especially when nobody is around to watch or distract them.
Pets have an amazing inherited skill, which allows them to chew up twenty stitches or staples in less than two seconds flat. By the time you realize it, it’s too late!
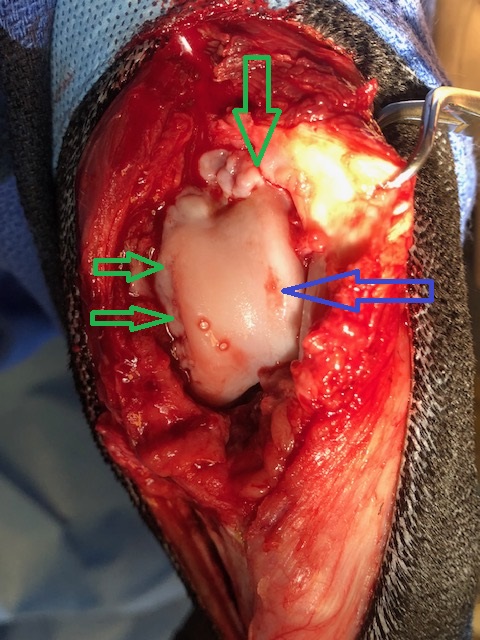
Below is an example of a dog who was caught in the act. She went home with a cone that is too short, and does not prevent reaching the incision. Clearly, the correct fit is critical.

I cannot begin to count how many times pet owners have asked me if their pet really has to wear an E collar.
And I cannot begin to tell you how many clients thought their pet was different, or well-behaved, or well-trained, or smarter, and didn’t need a cone.
Or how many pet owners were in tears after their pet chewed the incision open after they removed the cone “for only 5 minutes” or “just to give him a break” or “because she looked so sad.”
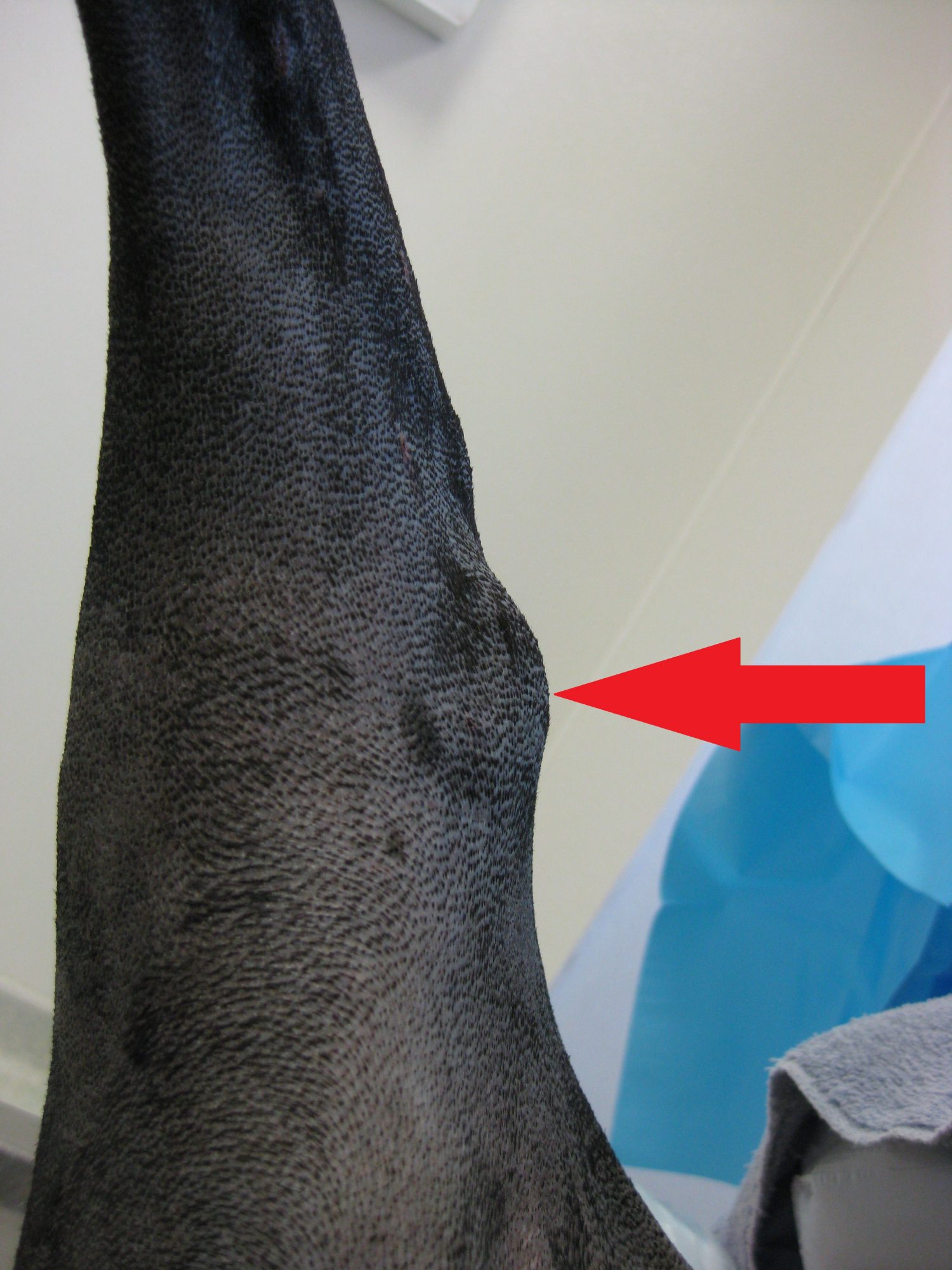
Below is a (mild) example of what happens when a pet licks the incision.

I cannot begin to add up all the extra money owners have paid to fix open incisions at their vet or the emergency clinic.
And I cannot tell you how many clients swear that they will not leave their pet’s side for 2 or 3 weeks. Meanwhile, I’m pretty convinced that these clients will need to sleep, or go to the bathroom, or get a bite to eat. There is no such thing as 24/7 supervision with a pet!
Depending on how bad the damage is, treatment may require rinsing the open area, cutting out damaged tissue and re-stitching the entire incision. For a little bit of perceived freedom from the evil cone, clients sometimes end up spending more money in anesthesia, surgery and antibiotics to fix an entirely avoidable problem, not to mention the discomfort the pet goes through – and a longer recovery. And ironically, then the pet needs a cone for even longer!
Below is another (mild) example of what happens when a pet licks the incision.

Leaving the E collar on at all times is the best way to get your pet used to it. If you feel bad for your pet and take the cone off, then put it back on when you leave, your pet may take it as a punishment and may try to remove or destroy it.
Patients can absolutely eat, drink, walk, pee, poop, and sleep with a cone on. In fact, the stricter you are with the cone, the quicker they will get used to it. In addition, pets do not hold grudges, so they will not be mad at you for being strict with the rules.
Collars are not to “shame” pets or annoy owners, they are essential for quicker and better healing of the incision. Call it a necessary evil or a cheap insurance policy. Next time your vet recommends an E collar or a similar device, please follow their advice. It truly is in your pet’s best interest.
Moral of the story?
The plastic cone is your pet’s best friend.
Any surgery has complications. Some are not predictable. Licking an incision is totally avoidable. We know how to prevent that. Please trust us, and please be part of the solution.
Your pet, in the end, will thank you for it.
What about alternatives to the plastic cone?
Marketers spend a fortune trying to convince pet owners that their alternative is better than the hard plastic cone.
There are soft cones, hard cylinders, foam “donuts,” inflatable “donuts,” various covers and sleeves and more.
As a surgeon, I have witnessed what seems like every conceivable complication.
Experience has shown me that these options are not as fool-proof as the standard plastic cone.
A stubborn or itchy pet will lick around a donut or soft collar, we see it all the time!
Bitter Apple or similar product may be placed around the incision – not directly on it. However, this does not deter some pets at all. Some actually love the taste!
So again, the hard plastic cone is your pet’s best friend… and the cheapest insurance policy against licking.
Phil Zeltzman, DVM, DACVS, CVJ, FF certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
10 ways to help a pet with arthritis
About 30% of cats and dogs are affected with arthritis.

Before we discuss 10 ways to help, please remember: arthritis cannot be assumed. It has to be proven (X-rays are one good way).
Giving anti-inflammatory drugs to your pet just because somebody “thinks” (s)he is affected by arthritis is just not appropriate. There is no cure for arthritis, but it can be controlled. Here are 10 ways to help…
1. Weight loss or weight control
Extra pounds add pressure on joints with arthritis. Losing weight is then critical. Your family vet can help your pet lose weight (with weight-loss food), or maintain the weight (with a “light” diet). One classic research study showed that “in overweight dogs, weight loss alone may improve lameness.”
It is important to remember that the front legs support 60% of the weight, whereas back legs carry 40%. Therefore, weight loss is even more important with arthritis in joints of the front legs: shoulder, elbow or wrist (carpus).
2. “Arthritis” diet
Once your pet has an ideal weight, you can switch to an arthritis diet. These diets are typically enriched in glucosamine, antioxidants (such as vitamins C and E) and omega-3 fatty acids (fish oil).
Such diets are perfectly balanced, i.e. they have all the necessary nutrients, vitamins and minerals, so they can be fed for life. However, they are not appropriate for a growing pet, so they should be used in adults only.
Pro tip: there is now a special food that help with weight loss (or weight control) and arthritis at the same time – a major improvement.
3. Joint supplements
Because there is never enough glucosamine or fish oil in any pet food, it is important to give supplements by mouth in addition. We will recommend them after most orthopedic surgery to manage the arthritis.
Other supplements can be injected by your family vet.

4. Controlled exercise
Lack of activity leads to muscle loss, a decreased range of motion in the joints, aka stiff joints, and weight gain (if you don’t decrease the calories).
Despite the discomfort, it is very important to continue exercising. Generally, slow leash walks are ideal. You can progressively increase their duration. For example, start with 5 minutes 2-3 times daily for one week, then increase that by 5 minutes each week.
These walks help keep muscles strong and joints flexible.
Supervised swimming, or walking in wet sand, or tall grass, are another great ways of providing low impact exercise, as long as your dog doesn’t struggle to get into or out of the water. Encouraging exercise in a cat can be challenging, but some owners are able to train their cat to walk on a leash!

5. Physical therapy (PT)
Even though untreated arthritis causses pain, not moving is only going to make thigs worse.
Physical therapy is a great, gentle wait to move joints in a controlled way.
Done at home or at a physical therapy center, PT can make a dramatic difference. Most doggie physical therapists (officially called rehabilitation practitioners) will perform some exercises that can only be done at their facility, such as walking in an underwater treadmill, and will show you exercises to do at home. PT starts with a “warm up” and ends with a “cool down.”
If you have ever needed PT for yourself, you may appreciate how dramatic a difference it can make in your pet’s life. I have personally seen rehab practitioners perform small miracles on some patients!
6. Anti-inflammatory drugs
The most commonly used pain medications used for arthritis pain are Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). Ideally used on an as-needed basis, rather than every single day, modern NSAIDs are safer and more potent than aspirin & “people” drugs. By the way, please never use people drugs in your pet without your vet’s complete approval, especially in your cat. Some of these drugs can be deadly.
Potential side-effects of veterinary NSAIDs include vomiting and/or diarrhea, with or without blood, lack of appetite, lethargy or jaundice (a sign of liver disease), or kidney disease. Your family vet will typically perform regular lab work, testing blood and urine, e.g. every 6 months or more often in at-risk patients, to monitor possible side-effects.
7. Pain medications
When anti-inflammatory drugs cannot be used, or are not strong enough, other pain killers can be given (gabapentin, tramadol etc.). There are other options, which need to be tailored to each individual patient. Sometimes, it is a matter of “trial and error” until the ideal drug combination is found. Every patient is different, so there is no ideal solution that works on all patients.

8. Environment changes
Many small tricks can help. Keeping your pet in a dry and warm place should help, just like it would help an arthritic person. It is important to keep your pet on thick, soft, clean padding at all times, rather than on tile or linoleum (although some pets seem to prefer those!). Minimize access to stairs. Elevate the food & water bowls.
If you have a few steps on your deck, you could build a ramp. Some companies sell steps to help pets get onto furniture more easily. To get in the car or the truck, you can also use a ramp. Whether inside or outside, always provide good footing so your pet doesn’t “do the splits”. Hardwood floors can be covered with area rugs or yoga mats. And be extra careful on ice during the winter time. Pets can get seriously hurt after slipping on ice. An easy solution is to use a sling under your dog’s belly.
9. Periodic re-evaluations
Follow up exams with your vet are critical to adjust the plan to your pet’s progress. For example, if you are trying to make your pet lose weight, monthly weigh-ins are important to track your progress. The amount of food may need to be adjusted, otherwise the weight may just plateau if you continue feeding the same amount.
Similarly, pain medications could be changed or the dosage adjusted depending on your pet’s progress.
10. Surgery
In some cases, surgery is an excellent way to treat arthritis. From simple procedures (removing a flap of cartilage or part of a bone) to more complicated surgeries (fusing a joint, or a total hip replacement), ask your family vet or your surgeon if your pet would benefit from surgery.
So there you go: there are (at least) 10 ways to help a pet with arthritis. There are other modalities, such as acupuncture and stem cell therapy, which you can discuss with your family vet or your surgeon.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
10 deadly sins of untreated ACL tears
Pet owners sometimes ask what would happen if we didn’t address a torn anterior cruciate ligament (ACL). Dr. Google and random people will suggest conservative treatment as a perfectly valid option.

A non-surgeon colleague even wrote elsewhere that since people often don’t need surgery for an ACL tear, then we shouldn’t need it in dogs. Respectfully, this shows a basic misunderstanding of the differences in functional anatomy between dogs and humans. Let’s mention two:
. Humans are straight legged. Dogs always have their knees flexed when standing.
. The human tibial plateau angle is somewhere around 7 degrees. Dogs’ tibial plateau angles vary from around 20 to over 60 degrees, with a back-of-the-envelope average of 24 to 28 degrees in most of my tibial plateau leveling osteotomy (TPLO) patients.
How many reasonable, objective, ethical, honest reasons can you find to recommend conservative treatment as opposed to surgery?
Here are 10 consequences of untreated ACL tears:
1. Pain
Patients with a torn ACL are in pain.
Please remember that limping or favoring or babying a leg = pain.
Pets are not crazy! Holding the affected leg up or limping hurts less than putting full weight on the leg.
When the tear becomes older, pain might subside to some degree, but it stills hurts.
Another reason patients are limping is because the knee is unstable or wobbly.
2. Arthritis
We routinely notice during surgery that patients with long-standing (chronic) ACL tears have more arthritis than patients with a recent injury. This, in turn, leads to pain.
Patients with partial tears typically have less arthritis than patients with complete tears. Recent tears also regularly lead to less arthritis than older (chronic) tears.
Therefore, the sooner we perform the surgery, the better for the patient.
3. Scar tissue
Scar tissue is what we rely on after conservative treatment for an ACL tear. Experience proves that scar tissue alone is not enough to provide good function, at least in medium- and large-breed dogs.
Scar tissue is manifested by what we call the “medial buttress,” which can be a very prominent bulge inside a pet’s knee.
In turn, scar tissue leads to our next point.
4. Decreased range of motion
A long-term consequence of arthritis and scar tissue is a decreased range of motion of the knee.
Patients with older (chronic) ACL tears commonly experience a decreased range of motion. This might not matter much to a couch potato, but it will affect the performance of an active family pet or a working dog.
5. Muscle atrophy
Patients who favor a hind leg classically show various degrees of muscle atrophy because of poor use of the leg.
This can be assessed easily by measuring the circumference of the thigh with a simple tape measure.
6. Exercise intolerance
Obviously, a family pet or working dog will have a tough time running around with a sore knee.
Dogs with a torn ACL are reluctant to play or go for walks. Exercise intolerance or poor athletic performance classically leads to weight gain, because these pets often receive the same amount of food (and sometimes more, along with more treats).

7. Weight gain
A consequence of many of the above changes is decreased activity, which invariably causes weight gain.
This is a common observation in ACL patients. Unless you decrease your pet’s food intake to match the decrease in activity, weight gain is inevitable.
8. Opposite ACL tear
Arguably, weight shifting may lead to a tear of the opposite ACL. While this might be manageable in a yorkie or a cocker, it becomes a much bigger problem with a Labrador or a mastiff. Helping a 100 lb dog who has both ACLs torn at the same time is not easy!
9. Tear of the meniscus
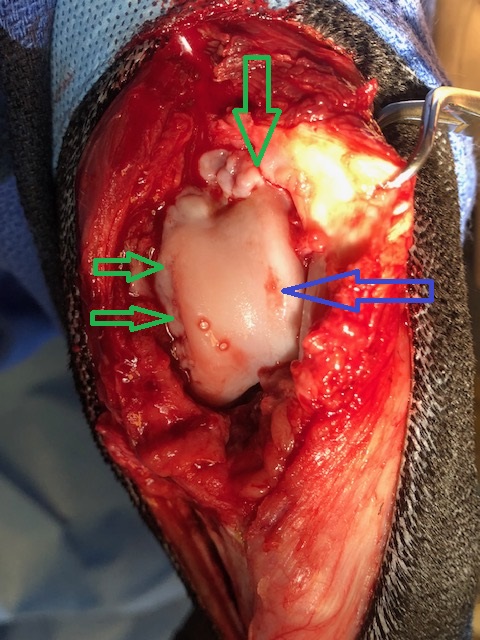
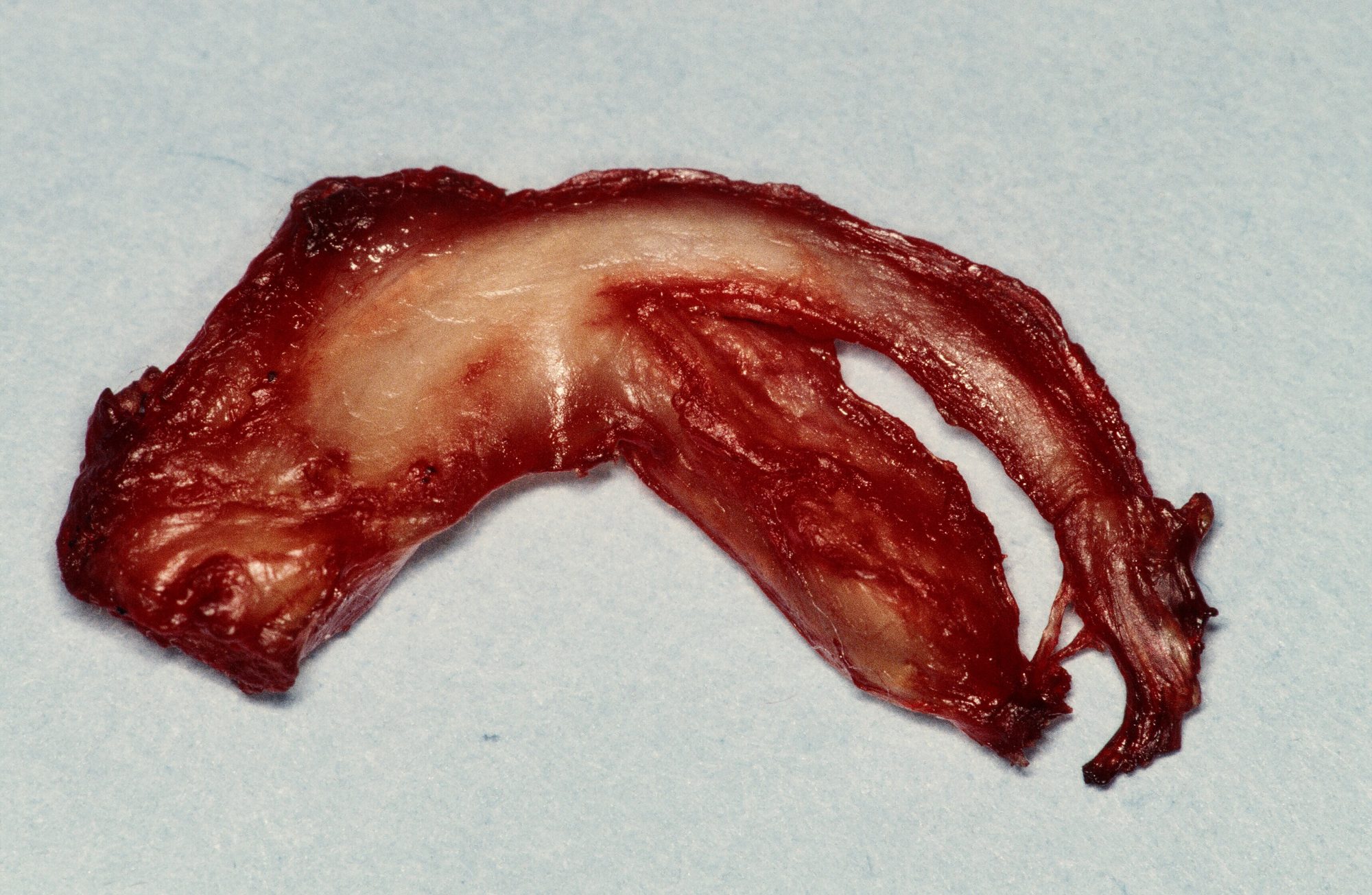
Instability in the knee can lead to a tear of the meniscus (see picture below), which is a pad of cartilage in the knee. This can cause even more pain.
On the opposite, once the knee is stabilized, the risk of a tear of the meniscus is minimized.
10. Distant problems
The changes in gait and posture can affect all three other legs, as well as the spine. Weight shifting may cause or exacerbate an orthopedic problem in another leg.
A doggie physical therapist told me once: “An ACL rupture is the beginning of a cascade of events in other body parts – joints, muscles – that we can’t forget.”
To a degree, some of the above changes can be used to “date” an ACL tear. From experience:
. A patient with a recent ACL tear classically is lame and painful.
A patient with an old (chronic) ACL tear typically presents with limping, pain, arthritis, decreased range of motion, muscle atrophy and weight gain. In surgery, we certainly see much more bone spurs in a dog with a chronic tear than with a recent tear.
From a surgeon’s standpoint, an ACL tear is a very fixable problem.
Sure, it is possible to live with a torn ACL. Certainly, it might be the only option if you absolutely cannot afford surgery.
ACL surgery has changed dramatically over the past few years. I now expect a return of at least 95 % of normal function in at least 95 % of my patients of any size after ACL surgery, of any type.
So it’s hard for me to believe that affected dogs, especially large ones, have (and will have) a good quality of life with an untreated ACL tear.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!