Dr. Phil Zeltzman’s Blog
Ninja, my biggest surgical & ethical challenge in 2021
“I beg you for help.”
Such was the subject line of the email.

In the email, a pet owner explained:
“My dog Ninja, a 6 year old Siberian Husky, just had a CAT scan, then surgery to drain a cyst in his enlarged prostate” (17 cm long – about 7 inches).
“Because of the pressure on the colon and the bladder, Ninja couldn’t defecate or urinate!”
“His bladder has been so over-stretched, that it couldn’t contract and now Ninja still can’t urinate. A urinary catheter was placed temporarily… and the only option the surgeon gave us was euthanasia!”
“I don’t want to put him down. He is eating, drinking and (now) pooping. He acts normal but can’t pee. Please help me, I am very desperate.”
Desperate times call for desperate measures.
Ninja had a condition similar to unfortunate older gentlemen who struggle to pee because of an enlarged prostate. It is a frustrating & painful situation. But in a dog, it can be life-threatening.
There is a better solution than euthanasia. I suggested a surgery that involves placing a special tube in the bladder and allows draining the bladder on demand.
It’s certainly not for every pet owner, but Ninja’s owners were exactly the right people for the challenge: dedicated, attentive, and totally in tune with their dog. They had done their homework and found out about this option by reading my blog about Madeline, who had the same surgery for a different problem (a bladder tumor).
Chapter 1
Time was of the essence, so we quickly scheduled surgery at Brodheadvsille Vet Clinic.
Ninja had a “cystostomy” surgery, where a tube was placed to drain the bladder through an opening in the skin.
In addition, Ninja was neutered. After that necessary step, male hormones would decrease and cause the prostate to shrink. That would reduce the pressure on the urethra and allow Ninja to urinate.
Chapter 2
Everything went according to plan for about a month… until Ninja accidentally stepped on the tube.
The logical next step was to replace the life-saving drain. Unfortunately, preop bloodwork showed some concerning changes. Ninja’s immune system was attacking his own red blood cells (hemolytic anemia) and platelets (thrombocytopenia). This double condition is called Evans’ syndrome.
So we changed plans. Since it was too risky to perform surgery with such low numbers of red blood cells and platelets, we placed a traditional urinary catheter to allow Ninja to urinate.
We were able to do this thanks to the generosity of another practice owner near Allentown, PA.
The catheter had to be changed frequently to lower the risk of bladder infection (UTI).
His faithful owners would drain the bladder multiple times a day to allow it to stay small. Remember, the bladder was so over-stretched, that it couldn’t contract anymore…

Chapter 3
At that point, Ninja was referred to a board-certified internist (a medicine specialist) to manage his Evans syndrome.
Meanwhile, Ninja still couldn’t pee!
To make matters worse, an ultrasound showed that the prostate now had an abscess. Again, euthanasia was recommended.
Again, his owner called me to see if there were any other options.
After reaching out to multiple specialists, we found one willing to help. My amazing nurse and I suggested a completely crazy plan:
. An ICU specialist at a specialty hospital in NJ accepted to let us use the key to our problem: a special transfusion with platelets to help with clotting.
. We would drain the abscess at another practice in NJ, and place a new cystostomy tube to allow Ninja to pee.
. We would recover Ninja under the supervision the ICU specialist.
Amazingly, Ninja’s owners decided to go with surgery, about 2 months after the first one.
The procedure was uneventful, and after 2 days in ICU, Ninja went home.
Then came weeks and months of amazing dedication from Ninja’s owners.
Long story short, Ninja progressively got better and stronger.
Then out of the blue, to everybody’s surprise, he started to pee on his own!
After agonizing over the right time to remove the tube, we eventually did, once we were convinced that Ninja was emptying his bladder on his own sufficiently to survive.
Now you understand why Ninja was such a technical and mostly ethical dilemma for me.
When should a surgeon stop helping?
When should a pet owner stop hoping?
When should a pet to cross the rainbow bridge?
Why did I choose Ninja’s story…
… over so many other amazing pet stories I was fortunate to play a part in in 2021?
Because of the number of people who played a role in Ninja’s survival.
In the middle of the COVID crisis, it was an absolutely astonishing display of generosity, love and care, by multiple vets and nurses.
Across half a dozen practices.
And across 2 States (PA & NJ).
(trust me, I gave you the short version!!!)
Everybody rallied behind Ninja, led by his loving owners.
And the result is one happy, playful, fluffy Husky, whose only wish is to be comfortable, to be able to pee, and to return his owners’ love.
Ninja’s owner created an amazing video summary.
It’s a story about the love of a family pet.
A story about the power of dedication.
A story about not taking no for an answer.
You can watch it here: https://vm.tiktok.com/ZMRatj6Co/
Fair warning: it’s a tiny bit emotional…
What’s the moral of the story?
1. Neutering early in life decreases or eliminates the chances of having prostate issues in male dogs. There are many other good reasons, which you can read about here:
/blog/top-10-reasons-to-neuter-your-pet/
2. You are your pet’s best advocate. If something makes no sense to you, don’t give up. Sadly, there is not a solution or a cure for every condition. But at least, you should explore your options.
Don’t take no for an answer. Get a second opinion.
This is exactly what Madeline’s and Ninja’s owners did. They didn’t take no for an answer, and they saved their dogs’ lives.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
How I got a chance to fix a baby coyote!
I recently had the unique opportunity to fix a 2 month old coyote baby!

One of my referral clinics is heavily involved in wildlife rehab.
Mama coyote had been hit and killed by a car.
Her two orphans were eventually found.
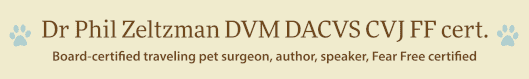
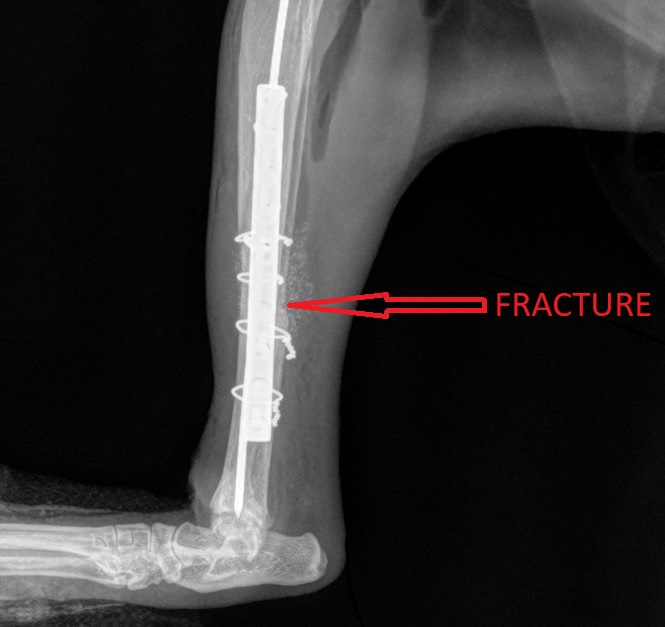
One pup, promptly named Lukas, had sustained a fracture of the right humerus, the bone in the arm, which required surgery.


Preop blood work showed that he was healthy enough to undergo anesthesia.
There were 3 main risks to be aware of:
. Surgery is challenging because of puppies’ bones are soft, so they don’t hold screws very well.
. Pediatric patients who undergo anesthesia are at risk for hypoglycemia (low blood sugar), hypothermia (low temperature) and hypotension (low blood pressure).
. It’s much tougher to rehab a wild animal than a tamed house pet.
Fully understanding the risks, we put baby Lukas under anesthesia.

What we couldn’t know before doing surgery, since scar tissue is not visible on X-rays, is how old the fracture was. It turns out that it had been a while. And that makes sense: by the time the terrified pup was found, rescued, assessed, transferred to the vet clinic, and then transferred to my care, it had been many days.
Another proof that the fracture was old is that his range of motion was very poor, even under full anesthesia (my exam notes said “Poor range of motion preop: cannot flex elbow beyond 45 degrees”).
My surgery report said “TONS of scar tissue… very difficult to recognize the anatomy of the bone.”
So we did what we could: stabilize the fracture the best we could, since lining up the bone was not possible. The result is not pretty on X-rays, but functional…

A stainless steel plate and 8 screws were placed.
Fortunately, Lukas recovered smoothly from anesthesia.

Despite the above challenges, the benefit of being young is that bones heal very quickly.
The next challenge was to allow Lukas to heal, confined in a small area, fed a healthy diet, while doing physical therapy so his elbow wouldn’t get too stiff.
All of that, while handling him as little as possible. It is very detrimental to overhandle wildlife, especially pediatrics, due to the risk of human imprinting.
Imprinting refers to a critical time in young animals when they form attachments and develop their identity. So they need to “imprint” onto their mother, or their siblings, or their buddies, not humans.
To avoid this risk, Lukas was eventually transferred to a rescue association.
Once fully healed based on 6 week X-rays, Lukas was reunited with his brother. They were kept at the rescue until they were 6 months old. Then they were released together, to live their coyote lives…
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Pain is not acceptable
As a surgeon, my goal is to eliminate pain as much as humanly possible.
Let’s go over a few stubborn myths related to pain in pets.

1. My pet doesn’t cry out
“My pet is not crying and therefore is not in pain” has to be one of the most stubborn myths vets face on a daily basis.
When a pet limps or favors a leg or doesn’t put full weight on a leg, they are most likely in pain.
When a pet’s activity decreases, they may be in pain.
When a pet’s routine or habits change, they might be in in pain.
When a pet’s appetite decreases, they could be in in pain.
The fact is, most pets, especially cats, do not cry out when they’re in pain. Of course, if you step on their foot, they will cry out in pain, but that is short-lived because of what we call acute pain. Long-term, ongoing, continuous, sustained pain is called “chronic” pain.
Similarly, a dog may cry out in pain when (s)he initially tears a ligament, such as an ACL. But then the pain becomes subtle or low-grade and there’s typically no more crying.
Yet as long as they’re limping, it means that pets are in pain.
It’s the same idea as when you have a pebble in your shoe. You will shift weight to the other leg to decrease the pain. But as long as you put weight on the foot with the pebble, there will be some degree of pain.
Pain in cats is even harder to assess than in dogs. Cast tend to change their habits: less grooming, less jumping up or down, decreased appetite, hiding, fewer interaction with humans, withdrawal.
2. My pet is just old
Age seems to be the catchall excuse for multiple ailments. For example, urinating in the house is often blamed on old age, even though a bladder infection or bladder stones ( /blog/?p=1841) might be present.
When it comes to a pet’s decreased athletic ability – unwillingness to play, using stairs or jumping on furniture – many pet owners believe that age is the culprit.
Before we get to that conclusion, it’s important to make sure your pet doesn’t have a torn ACL, or severe hip dysplasia, or a bulging disc.

3. Pets don’t feel pain like we do
Some people still think that pets don’t feel pain like we do. Yet mammals have the same type of nerve endings, pain pathways and pain perception center in the brain as humans do.
To think that an animal in pain doesn’t deserve the same kind of treatment as humans is simply wrong.
4. There’s nothing we can do
Some pet lovers are told that because one pain medication doesn’t seem to work anymore, there are no other options.
Yet there are almost always other options: other pain meds, surgery, physical therapy, acupuncture, weight loss etc.
If all options have truly been explored, then maybe it’s time to have a discussion about quality of life, but not until then.
When the end finally does come around, you can rest assured that you truly did everything possible.
5. Postop pain is beneficial
Vets used to say that postop pain is a good thing because it keeps pets quiet, and that helps prevent injury to the surgery site.
We now have a much better understanding of the implications of untreated pain.
In my surgery practice, we routinely use 4-6 different techniques to prevent and treat pain. The drugs and techniques are well known, it’s just a matter of using them.
6. Minor procedures don’t need pain medication
This is another stubborn myth. Even what seems like a minor procedure, like a neuter, a mass removal or a tooth removal causes pain and should be treated.

7. Pain medication in old or sick patients is dangerous
There are multiple pain medications we can choose from. Each drug has potential side-effects, for example related to the kidneys and the liver.
This is a manageable risk. It’s a matter of pros and cons. We can easily monitor consequences on kidneys and liver with regular bloodwork. In a healthy pet on an anti-inflammatory, bloodwork is typically recommended every 6 months. In a pet with kidney or liver issues, bloodwork can be performed every 3 months, or even more often.
Another strategy is to decrease the dose of “risky” medications, usually an anti-inflammatory, or stop it altogether. We can also replace it with other, safer pain medications.
8. My client won’t pay for that
Some vets are concerned that you can’t afford proper pain prevention and treatment.
There, I said it.
If that is your case, then you should discuss it honestly with your vet.
If not, then you should demand the best possible pain management for your pet.
9. Surgery causes pain
A few of my clients have declined surgery for this reason.
As a surgeon, I’m not naïve enough to ignore the fact that left untreated, pain will occur after surgery. Again, most of my patients benefit from half a dozen pain management techniques.
This includes IV medications, special IV fluids, local pain meds, pain medications by mouth, pain medication injected directly into joints, pain medication injection around the incision etc.
So being fearful of surgery because of the fear of pain does not make sense. We can prevent and treat pain. In fact, a common reason to do surgery is specifically to treat pain.
Think of a broken leg. One consequence of surgery is to decrease the pet’s pain.
So it is quite the opposite: surgery helps decrease pain and eventually, it eliminates it.
10. My pet is not in pain
With all due respect, I would argue that many pet owners do not realize how much pain their pet is before surgery. Why is that? Possibly because everybody (humans and pets) slowly got used to it.
Case in point, we recently did a Total Ear Canal Ablation (TECA) in a Cocker with severe ear infections.
TECA is a pretty invasive surgery that has a reputation for being painful. So we use as many pain medications as possible, as mentioned above.
The very next day, the owner sent an email with an update: “He had a few rough moments trying to get comfortable. But once we got him to take his pain medication, he fell asleep and slept through the rest of the night.
(…) He woke up like a new dog today!
You would never even guess he had surgery. He had a full appetite, and is walking around very alert and actually attempting to play which we are trying to discourage at this point.”
Keep in mind, this comment came from a very smart, attentive and loving pet owner. She is very in tune with her dog. She was surprised by how comfortable her dog was after such an invasive surgery and went out of her way to email me to acknowledge how much pain her dog must have been in before surgery. And how comfortable he was after surgery.
This is actually one of vets’ biggest frustrations. We know when a pet is in pain and it’s sometimes difficult to convince a pet owner that their pet is in pain.
By the same token, if you feel that your family vet does not believe you that your pet is uncomfortable or painful, then it is your absolute right to seek a second opinion until you find somebody who takes you seriously (here is a perfect example: www.drphilzeltzman.com/blog/joshuas-story-taking-pain-seriously).
As I always say, “pain is not acceptable.”
We are extremely fortunate to have access to all kinds of pain medications and surgery options to make many pets more comfortable.
Here are 20 signs that your pet might be in pain
. Limping, favoring a leg
. Decreased social interaction, withdrawal
. Anxious facial expression
. Submissive behavior
. Decreased movement
. Decreased jumping (eg on the sofa, in the car)
. Difficulty doing stairs
. Decreased grooming
. Whimpering
. Howling
. Growling
. Guarding behavior (e.g. head shy)
. Aggressiveness, biting
. Decreased appetite
. Weight loss
. Self-mutilation (licking, chewing, biting an area)
. Changes in posture
. Dogs: constipation
. Cats: Changes in urinary/defecation habits
. Hiding
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
How risky is it to anesthetize super young pets?
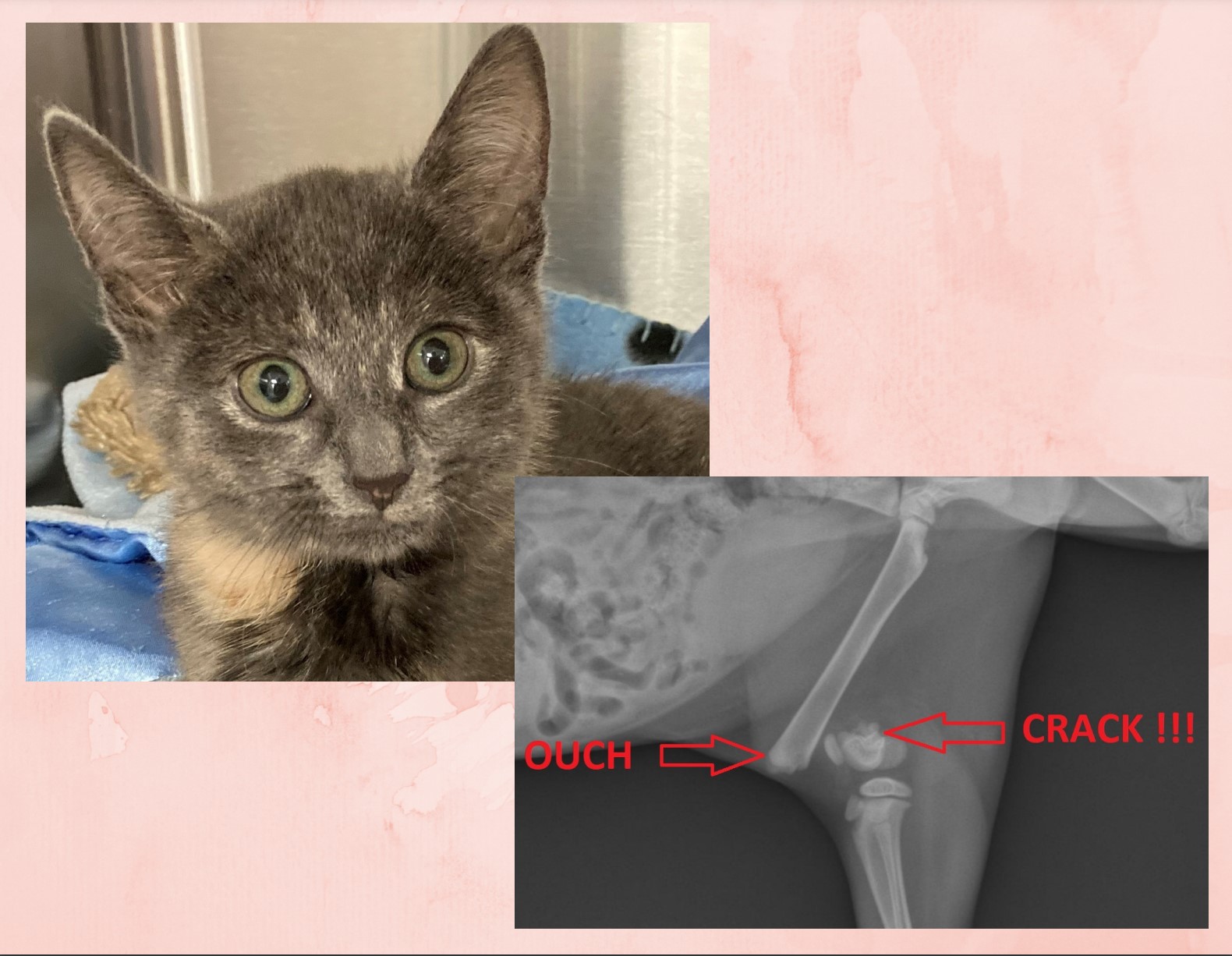
Rosalina, a 3 month old kitten.
Lukas, a 2 month old coyote.
Pup, a 3 WEEK old puppy.

What do these tiny patients have in common? They all needed a broken bone repaired. And they all super young.
Rosalina the kitten had a broken femur (thigh bone).
Lukas the coyote had a fractured humerus (arm).
Pup the puppy had a broken tibia (shin bone).
Their surgery was definitely challenging because of their soft bones. But the biggest challenge is really anesthesia.
Why is the risk of anesthesia in pediatric patients higher than in other patients?
Younger patients are at risk for hypoglycemia (low blood sugar), hypothermia (low temperature) and hypotension (low blood pressure).
Hypoglycemia
Younger patients have very little body reserves on board. So they are at risk for hypoglycemia (low blood sugar).
Patients who are old enough are often fasted at 8 pm the day before anesthesia.
In young puppies and kittens, we can’t do that, precisely to prevent hypoglycemia. Babies are typically allowed a small meal the morning of surgery.
Their blood sugar should then be monitored before, during and after anesthesia. If it’s too low, we can give sugar IV (in the form of dextrose) or by mouth (in the form of Karo syrup).

Hypothermia
Another struggle is keeping very small patients warm. All patients rapidly loose body heat under anesthesia. Super young patients are an even bigger challenge.
Of course, the solutions are well-known: warm air blankets, warm water blankets, IV fluid warmers etc.
These warming devices actually need to be put in action early and systematically to keep your pet safe.

Hypotension
Our pediatric patients may also have trouble with low blood pressure as a side effect of anesthesia.
Low blood pressure can be very dangerous if not corrected. Blood needs to appropriately move through the body to carry oxygen to all vital organs, such as the kidneys.
Decreased oxygen makes just about everything unhappy. It’s so important, that we monitor all of our patients’ vitals, including blood pressure, so changes can be identified early and corrected.
Blood work
Another way to decrease the risk of anesthesia is to run blood work. This helps us ensure that vital organs like the kidneys and the liver are healthy, and your baby can safely go under anesthesia. Of course, this applies to adults as well, and especially to seniors.
If the blood work does uncover an abnormality, it does not necessary mean that surgery will be canceled. However, it will often mean changing the anesthesia medications & postop pain medications used.
One specific thing we look for in young patients is abnormal numbers that could indicate an important condition called a liver shunt.
None of this information should change your mind about doing surgery. What it should do is educate you to make sure you and your vet can come up with the best plan for your baby, with the safest anesthesia and the smoothest recovery possible.
Hypoglycemia, hypothermia and hypotension are pretty straightforward to prevent when you are working with an experienced team. So don’t be shy about asking questions, so your super young pet is safe during anesthesia and surgery.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Who on earth wants surgery on their 23 year old cat?
I recently repaired a fracture on a 23 year old cat. Some of my nurses aren’t even that old! It’s a true story with a very happy ending.
Basil, the 23 year old cat, had a broken tibia. The shin bone was broken in 3 main pieces. He went to the local ER, where his owner was told that he was too old and should be put to sleep.

That did not sit well with Basil’s owner. He may be 23 years old, but he was healthy otherwise, so why end his life? His owner contacted me regarding Basil’s situation. We agreed that it was ethical to perform surgery on him, since he was healthy otherwise, and we scheduled him for surgery.

Fixing the shattered bone required 1 pin, 1 plate, 4 wires, and 9 screws to repair! A bone graft was added to speed up healing. Surgery went well and sweet Basil recovered smoothly under the close supervision of his nurses.
At home, he was strictly confined for 8 weeks. At suture removal, after only 2 weeks, he surprised everybody by walking around using the leg very well.
And after 8 weeks, follow up X-rays showed that the bone had healed nicely and we could start to increase Basil’s activity.

And after one more month of that, Basil returned to his normal Grandpa life.
So what’s the moral of this story?
As I always say, “Age is not a disease.”
A few conditions need to be met for surgery to be a valid option in my opinion:
. The patient should be reasonably healthy
. The condition should be fixable.
. Quality of life should be good after surgery.
. The owner should be 100% on board.
Two months after surgery, Basil’s owner writes: “My sweet 23 year old cat is finally back on the couch with me. He is getting giant hugs. He’s really doing great. I really have no words to thank you enough.”
I don’t see why we should deny help to a patient who fulfills these criteria.
Basil’s owner certainly felt that way, and I am sure Basil did as well…
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!